Digital Integrated Operating Room (Digital OR)
A non‑technical, long‑form guide to the definition, history, core building blocks, real workflows, planning checklist, pros/cons, and market landscape.
Cornerstone Knowledge Blog • Educational (no sales pitch) • Last updated: December 25, 2025
Table of Contents
- Introduction
- Digital OR Basics
- How a Digital OR Works
- Workflows in Real Life
- IT & Reliability Basics
- Planning & Implementation
- Market Landscape
- Pros, Cons, and “Poor Maintenance” Scenarios
- Common Mistakes (and how to avoid them)
- How to Choose the Right Scope
- Future Trends
- Terminology Glossary
- FAQ
- Summary
- References & further reading
1) Introduction
Operating rooms increasingly rely on video, imaging, and digital documentation. But in many hospitals, the information is scattered: one screen for the endoscope, another for patient monitoring, another computer for imaging, and separate tools for recording and teaching.
A Digital Integrated Operating Room (often shortened to “Digital OR”) is an attempt to bring those parts into a single, predictable workflow—so teams can focus on the procedure, not on “which cable goes where.”
2) Digital OR Basics
2.1 What it is (and what it is not)
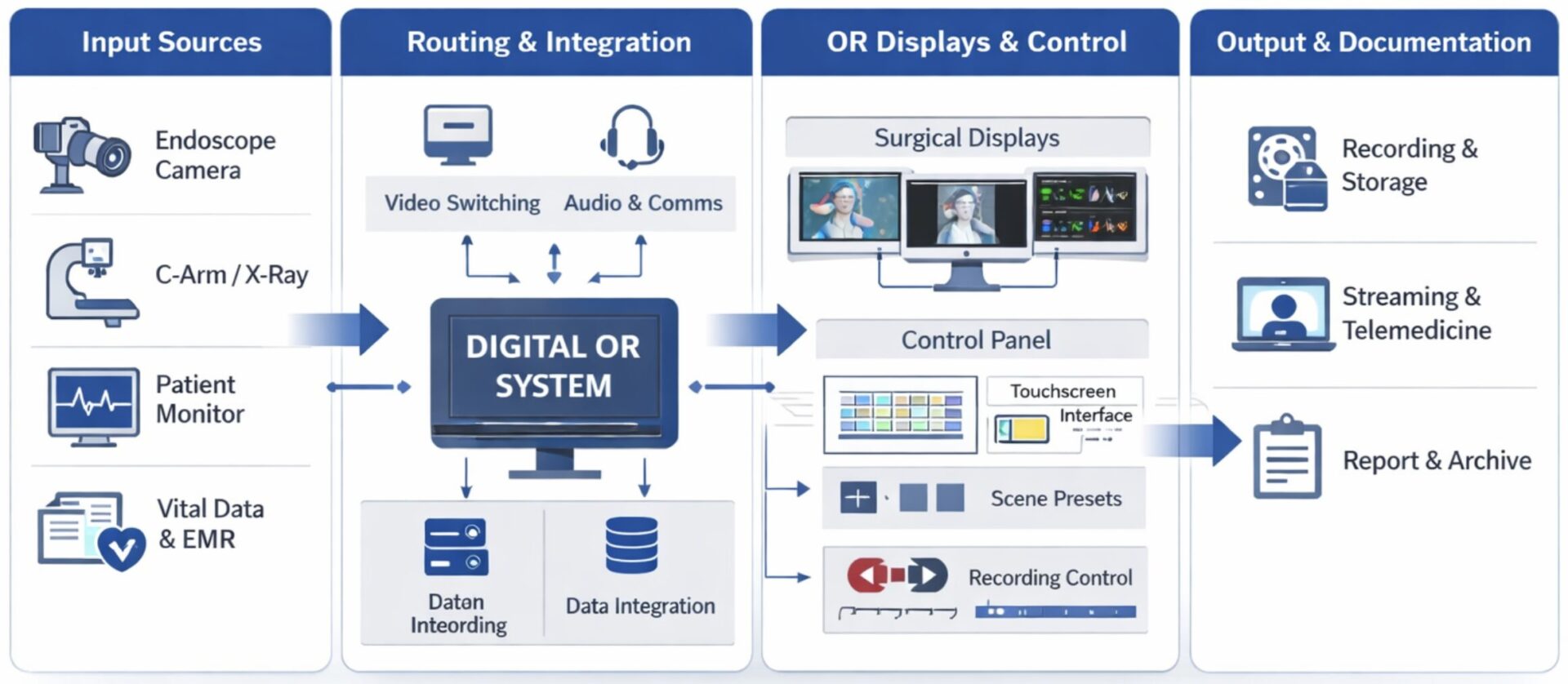
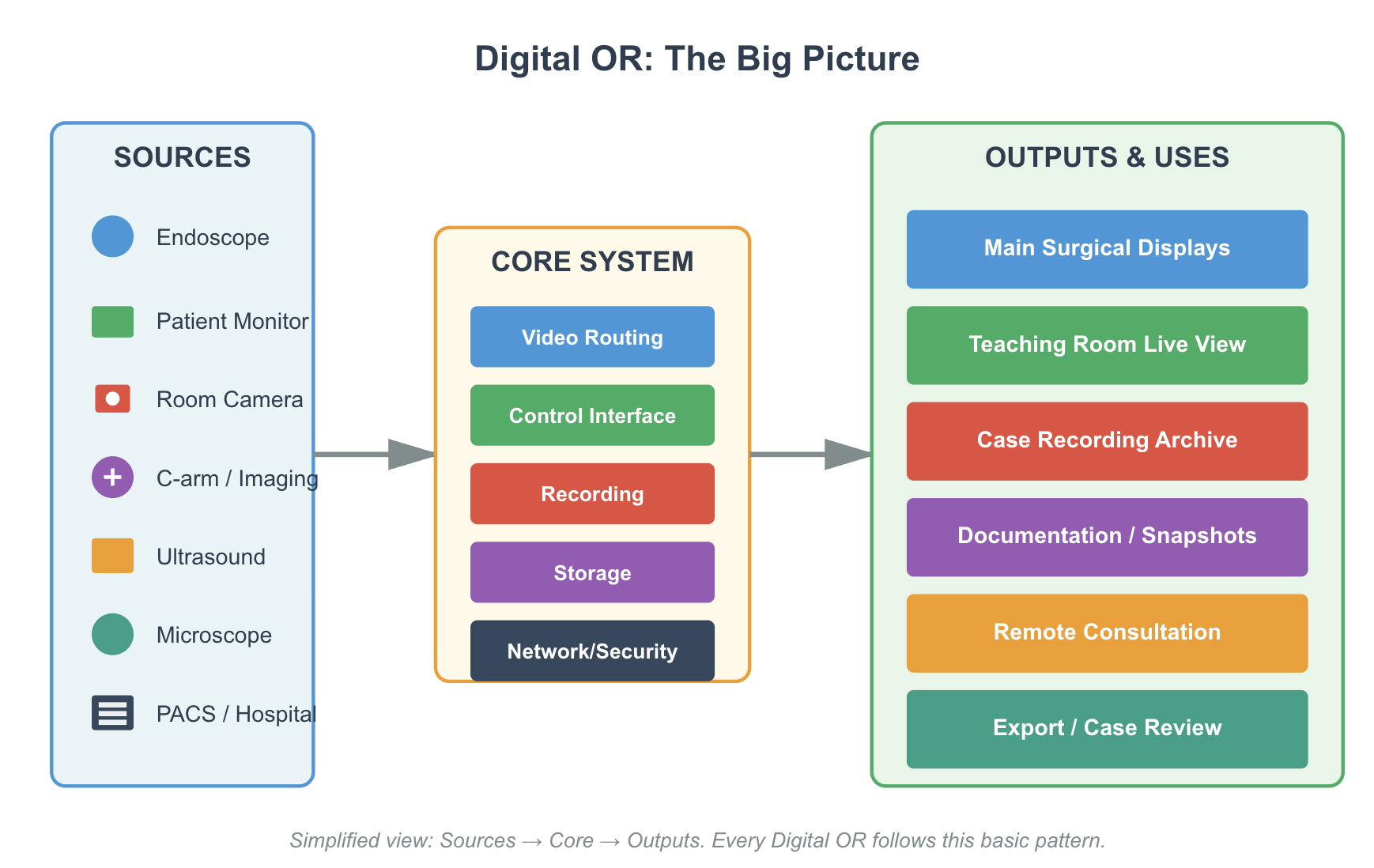
Simple definition: A Digital OR is a system that helps an OR team view, switch, record, share, and manage surgical video and information sources from a centralized interface.
What it is
A coordinated setup of sources (endoscope, cameras, monitors), displays, switching, recording, and (optionally) device control and hospital connections.
What it is NOT
Not a surgical robot. Not “AI surgery.” Not only a big screen. And not always a hospital-wide IT project (it can start with one room).
2.2 Pain points it solves (real OR situations)
Digital OR is easiest to understand when you link it to the everyday problems OR teams face. Below are common pain points (and what the system changes in real practice).
Neck fatigue & “blind angles”
In a traditional OR, surgeons often turn their head to view an endoscope monitor placed in a corner. A Digital OR can route any source to the best “front-view” display, reducing awkward posture and improving situational awareness.
Cable “spider-web” chaos
Temporary cables on the floor create clutter, trip risks, and constant plug/unplug errors. With structured routing (in-wall / boom / cabinet), signals enter the control core cleanly and are distributed logically to displays and recorders.
Slow switching & miscommunication
“Which input is this?” delays happen when staff must manually switch monitors or move devices. A Digital OR provides simple source selection and presets (scenes), so the team can change layouts quickly and consistently.
Recording is difficult or unreliable
Without an integrated recorder, teams use ad-hoc solutions (phones, external recorders, or nothing). A Digital OR enables consistent recording/snapshots with clearer file organization—assuming governance is defined.
Teaching & case review limitations
Training hospitals need stable live viewing (teaching room) and structured replay. Digital OR workflows make it easier to share the right feed at the right time with basic permissions and auditing.
Access to imaging inside the room
Teams may need CT/MRI/X-ray images during surgery. A Digital OR can support viewing from PACS (DICOM) or from approved local sources, reducing “leave the sterile area to check images” scenarios.
Inconsistent setup across shifts
Different staff may connect devices differently or choose different layouts. Presets (“scenes”) and standard routing reduce variation and make daily workflow predictable across shifts and rooms.
Troubleshooting takes too long
When something fails, teams often don’t know where to start. A good Digital OR includes clear labeling, basic status indicators (signal/record/storage), and simple logs so problems are solved faster and with less stress.
Slow OR turnover and room reset
Unplugging/rewiring between cases wastes time and creates mistakes. Clean structured routing and defined default presets shorten turnover and reduce “last-minute” switching chaos.
Recording creates compliance pressure
Recording is valuable, but uncontrolled export can create privacy risk. A practical system supports basic permissions and auditing so hospitals can benefit from documentation without losing control.
2.3 History & development timeline
Digital OR systems evolved as OR video became more important and more complex.
Era 1 — Standalone devices and analog video
Each device came with its own monitor and controls. Video sharing existed, but it was often messy: adapters, manual switching, and inconsistent quality.
Era 2 — Early integration (basic switching + wall displays)
Hospitals began to centralize video signals so the team could choose what appears on a main display. This reduced clutter and improved teamwork.
Era 3 — Recording, teaching, and remote viewing
As training needs grew, OR video recording and “teaching room” viewing became common. Hospitals started to formalize how cases are recorded, stored, and shared.
Era 4 — Workflow, permissions, and management
Modern systems focus on usability (one-button actions), roles/permissions, and keeping the whole setup stable over time (updates, logs, support).
3) How a Digital OR Works
3.1 The 3 layers of integration (video / control / data)
Think of Digital OR integration as three layers. Many misunderstandings disappear when teams use this model.
| Layer | In plain language | Typical examples |
|---|---|---|
| Video layer | Move images from sources to the right screens. | Endoscope → wall display; monitor → PIP; C‑arm → teaching room |
| Control layer | Operate devices in a consistent way (optional). | Room camera control; light/table interfaces; “scene” presets |
| Data layer | Record, organize, search, and share information safely. | Case recording; patient folders; export permissions; audit logs |
3.2 Core building blocks (explained simply)
Most Digital OR systems are built from the same ingredients. The difference is packaging, commissioning, and maintenance.
5.1 Sources (what generates the signals)
- Endoscope camera system (often the main video source)
- Surgical field camera (overview)
- Room/panoramic camera (teaching / documentation)
- Patient monitor (vitals output)
- C‑arm / ultrasound / microscope (by specialty)
5.2 Switching / routing (how the system chooses “what goes where”)
Switching is like directing traffic: the system decides which source appears on which screen. Multi-view layouts like PIP or side-by-side are common.
5.3 Displays (where the team watches)
Displays can be a main wall display, near‑patient displays, boom displays, or teaching room displays. Choose based on workflow, not only size.
5.4 Control interface (how humans operate it)
This is often a touch panel, in-wall console, or workstation. For non‑IT users, the interface should feel like: select source → choose layout → record → save/export.
5.5 Recording & storage
Recording can be local (inside the room) or centralized (server/NAS). Local recording is easier to start, but governance is more important.
5.6 Audio for teaching / communication
Teaching and conferencing work best when audio is planned properly (microphones, echo control, clear control roles).
3.3 Standard BOM checklist (vendor-neutral)
This is a practical, vendor-neutral BOM checklist for a “standard” Digital OR. Not every project needs every item on Day 1, but these are the most common building blocks.
| BOM Item | What it does (short) | Notes / options |
|---|---|---|
| Central cabinet / rack | Houses the system core (routing, recording, power, network) | Prefer front-service access; plan ventilation & cleaning |
| Video routing core | Selects and distributes sources to displays | Matrix-based or AV-over-IP; match port count to sources + future growth |
| Encoders / decoders (if IP-based) | Convert video to/from network streams | Useful for multi-room distribution; needs correct network design |
| Recorder (video + snapshots) | Captures procedure video and still images | Define channels, codec, resolution, and retention policy |
| Storage (SSD/NAS) | Stores case media files | Local SSD is simple; NAS adds governance but depends on network stability |
| Control interface (touch/workstation) | UI to choose sources, layouts, record, review | Presets (“scenes”) are critical for low-skill environments |
| Main surgical displays | Primary viewing screens (wall/boom) | Placement & line-of-sight matter more than maximum size |
| Aux displays (optional) | Extra displays for anesthesia, nursing, teaching | Improves teamwork if planned with roles in mind |
| Source input interfaces | Interfaces for endoscope, monitor, C-arm, ultrasound, etc. | Plan HDMI/SDI/DP; define an approved adapter strategy |
| Signal conversion & isolation (as needed) | Stabilizes compatibility and safety between devices | Medical isolation / grounding strategy may be required by local standards |
| Room camera (optional) | Overhead/panoramic view for teaching/documentation | PTZ camera helps teaching but needs simple presets |
| Audio (optional, but key for teaching) | Microphone + speaker for teaching/conferencing | Audio is where “teaching projects” often fail if ignored |
| Network switch | Connects system devices; required for IP video | Managed switch + VLAN if hospital IT requires segmentation |
| Time synchronization (NTP) | Keeps timestamps correct for files and logs | Small item, big impact on case tracking |
| User login / permissions | Controls who can record/export/admin | Essential if export is enabled; supports auditing |
| UPS / power conditioning | Improves stability during power events | Highly recommended in emerging markets |
| Structured cabling + patch panel + labeling | Prevents plug/unplug confusion and reduces downtime | Labeling + port map = “hidden ROI” for maintenance teams |
| As-built documentation set | Service guide for future troubleshooting | Include wiring diagram, port map, presets list, acceptance checklist |
| Service toolkit / spare kit | Fast recovery for common failures | Critical cables + adapters + spare SSD + fuse set (example) |
4) Workflows in Real Life
Workflows & use cases (with step-by-step examples)
Different vendors use different names, but these are the common capabilities that most projects care about.
6.1 Multi-source preview & switching
Operators can see sources and decide which signal goes to the main display(s).
6.2 Multi-view layouts
Common layouts include: single full screen, picture‑in‑picture, side‑by‑side, or quad view.
6.3 Case recording & snapshots
Recording can be one channel or multiple channels. Snapshots (still images) are commonly used for teaching and documentation.
6.4 Media management
Many systems organize recordings into case folders and provide basic searching and exporting.
6.5 Teaching & conferencing
Live viewing in a teaching room is common. Some projects also add annotation, time‑shift replay, or remote conferencing.
4.2 Step-by-step workflow examples
If your team can execute these workflows easily, the Digital OR is “working.”
Workflow A: Show endoscope + vitals on the main screen
- Select the endoscope source and send it to the wall display.
- Enable PIP view and choose the patient monitor as the PIP source.
- Save as a preset if the same setup is used every day.
Workflow B: Switch layouts during surgery
- Start with endoscope full screen.
- When needed, switch to a split view (endoscope + C‑arm / ultrasound).
- Return to the default view with one touch (preset).
Workflow C: Record a case + capture snapshots
- Confirm storage is available (a simple “green check” is ideal).
- Tap Record at the right time.
- Tap Snapshot when key events happen.
- Stop recording and confirm it is saved under the correct case folder.
Workflow D: Find a case and export it (under policy)
- Search by date / room / patient ID / procedure (as policy defines).
- Open the case file list (video + snapshots).
- Export only if policy allows it (some hospitals require supervisor approval).
Workflow E: Teaching room live view + time‑shift
- Teaching room selects a live feed from the OR.
- If allowed, pause/rewind locally (time‑shift) while the OR continues live.
- Use a microphone discipline rule: one person speaks at a time.
Workflow F: Remote consultation / MDT
Remote collaboration is possible, but needs stable network, defined permissions, and rules about what can be shared.
4.3 “Scenes” and device control (what’s realistic)
Some Digital ORs also control devices and room environment. Be realistic: not every device integrates cleanly, and not every hospital needs deep control.
8.1 What device control often includes
- Room/panoramic camera control (PTZ, presets)
- Basic room “scene” presets (routing + layout + camera preset)
- In advanced systems: lighting and table interfaces (depends on brand compatibility)
8.2 Why “scene control” matters
A “scene” is a preset that bundles multiple actions. For low-skill environments, presets reduce mistakes dramatically.
4.4 Recording, export, and governance (what hospitals must decide)
Recording is powerful—but it creates responsibility. Before enabling recording and export, align with hospital policy.
9.1 Decide what to record
- Endoscope feed only?
- Endoscope + surgical field camera?
- Also vitals? (some hospitals avoid including identifiers on screen)
9.2 File naming and case folder logic
A simple rule wins: one case = one folder. Inside: recordings + snapshots + notes. The folder name should match policy (date + OR + patient ID or anonymized code).
9.3 Export rules (USB / network)
USB export is convenient, but increases privacy risk. Consider at least: user login & permissions, audit logging, and (if required) encryption/watermarking.
5) IT & Reliability Basics
5.1 PACS/DICOM and hospital connections (plain language)
IT integration is where people get intimidated. The truth is: you can stage it.
10.1 PACS / DICOM
PACS is the hospital’s image library (CT/MRI/X‑ray). DICOM is the standard used to store and move those images.
10.2 HIS/EMR
HIS/EMR systems hold patient records. Some Digital OR projects integrate patient lists for better case organization (often a “Phase 2” item).
10.3 HL7
HL7 is a hospital messaging standard. You don’t need to learn HL7 to plan scope—just decide if automatic patient list sync is needed.
5.2 Network basics, cybersecurity, uptime, and troubleshooting mindset
The best Digital OR is the one that works every day. Reliability beats “one more feature.”
11.1 Roles and permissions
Many systems use role levels such as Admin / Normal user / Guest. This reduces mistakes and controls data export.
11.2 VLAN in one sentence
A VLAN is a way to separate OR traffic from other hospital traffic, improving stability and security.
11.3 Updates, logs, backups
- Updates: who approves them, and how often?
- Logs: how to capture logs when something fails (for remote support).
- Backups: if recordings matter, where is the backup?
6) Planning & Implementation
6.1 Installation + commissioning checklist
A Digital OR is not only “equipment.” It is also space, cabling, power, and a commissioning plan.
12.1 Space & placement
- Where is the rack/cabinet located (in-wall / technical room / boom)?
- Where do staff stand when using the control panel?
- Is the placement hygienic and easy to clean?
12.2 Cabling pathways
Plan cable routes early: video, control cables, network, and power. Good pathways reduce future service headaches.
12.3 Power, grounding, EMI reality
OR environments include devices like electrosurgical units (ESU). Power stability, grounding, and EMI considerations should be included in acceptance testing.
12.4 Commissioning & acceptance testing
Write an acceptance checklist that matches your workflows (Section 7). If the team can pass those steps repeatedly, the system is ready.
6.2 Levels of Digital OR (Level 1 → 4)
A staged approach is safer than starting “everything” on Day 1. The table below maps typical capabilities to the BOM building blocks you should expect at each level.
| Level | What you can do | Typical BOM blocks included | Who it fits best |
|---|---|---|---|
| Level 1 — Basic Video Integration | Show the right source on the right screen; simple switching | Central cabinet/rack; video routing core (basic); main surgical display(s); source inputs (HDMI/SDI/DP plan); structured cabling + labeling; power protection (recommended) | New ORs that want clean daily AV workflow with minimal complexity |
| Level 2 — Recording & Case Files | Record video + snapshots; basic case folder management; simple review | Everything in Level 1 + recorder; storage (local or centralized); control interface (touch/workstation); basic user roles (recommended); time sync (recommended) | Hospitals that need teaching/documentation basics without heavy IT dependence |
| Level 3 — Teaching & Collaboration | Teaching-room live viewing; conferencing (optional); room camera workflows | Everything in Level 2 + teaching room display(s); encoders/decoders (if multi-room/IP distribution); room camera (optional but common); audio (mic/speaker); network switch (managed if IP video) | Teaching hospitals and training centers where sharing workflows is a daily need |
| Level 4 — Hospital IT Integration & Central Management | PACS/HIS integration; centralized archives; unified accounts; multi-room governance | Everything in Level 3 + PACS/DICOM viewing integration approach; HIS/EMR interface (if required); centralized storage/NAS; audit logs; stronger access control; cybersecurity segmentation (VLAN); backup strategy | Hospitals with strong IT support, policies, and long-term operational ownership |
6.3 Digital OR vs. Digital Surgical Department
Digital OR (one room)
Focus: make one OR’s video, recording, and workflow stable and easy. It can be largely standalone and still deliver value.
Digital Surgical Department (many rooms + central management)
Focus: manage multiple ORs—shared video distribution, centralized archives, unified accounts, standardized workflows across rooms.
7) Market Landscape
7.1 Key players by region (China / Europe / USA / Japan / others)
7.2 Mini-table: each player’s strength focus
Digital OR projects usually combine multiple player types. Knowing the ecosystem explains why outcomes differ across hospitals.
7.3 Player types (ecosystem)
OR integration suites
End-to-end systems combining video, control, recording, and workflows (often premium).
Video-over-IP & visualization
Infrastructure moving video across rooms (the “pipes and pixels”). Often vendor-neutral.
Endoscopy/device ecosystems
Devices central to OR video (endoscopy, lights, tables). Integration depth varies.
Data/workflow platforms
Focus on documentation, analytics, governance, interoperability.
Local system integrators
Installation, commissioning, training, support. Often decide success/failure.
Component suppliers
Displays, capture, encoders, cabinets, audio—used inside custom solutions.
7.4 Representative examples (not a complete list)
Availability varies by country. Always confirm regional portfolio and support.
| Player | Region | Type | Strength focus (simple wording) |
|---|---|---|---|
| Stryker (OR Integration) | USA / Global | OR integration suite | End-to-end OR integration ecosystem |
| Getinge (Tegris) | EU / Global | OR integration suite | OR integration + device/room operation + data/video integration |
| KARL STORZ (OR1 portfolio) | EU / Global | OR integration suite | Workflow + multi-device control + communication |
| STERIS (OR Integration) | USA / Global | OR integration suite | Integration options + perioperative ecosystem |
| Olympus (room/procedure integration) | Japan / Global | Visualization + integration | Procedure-room visualization + integration approach |
| EIZO (CuratOR) | Japan / EU presence | Video mgmt + OR panels | OR wall panels + video-over-IP management + surgical displays |
| Barco (Nexxis) | EU / Global | AV-over-IP platform | Uncompressed high‑resolution AV-over-IP distribution |
| Richard Wolf (core nova) | Germany / Global | OR integration suite | Device operation from OR workstations + media management |
| Merivaara (OpenOR) | Finland / EU | Modular integration | User-friendly integration for varied hospital tiers |
| Skytron (video/OR integration) | USA | OR integration | Practical integration offerings |
| Mindray (MR‑DOR / OR solutions) | China / Global | Digital OR vendor | Digital OR systems + broader perioperative portfolio (varies by region) |
| Caresyntax | USA / EU | Data/workflow platform | Vendor-neutral surgical data integration + analytics focus |
7.5 How to evaluate “real capability” (educational checklist)
- References: real installed sites in your region?
- Service model: who commissions, trains, supports after handover?
- Governance: roles/permissions/audit/export policy clear or vague?
- Upgrade policy: how are updates handled without disrupting OR schedules?
- Spare parts: critical parts stocked locally?
8) Pros, Cons, and “Poor Maintenance” Scenarios
8.1 Benefits (clinical + workflow + training)
- Team coordination: right source on the right screen.
- Teaching: live viewing and replay for training.
- Documentation: recordings/snapshots enable review and improvement.
- Standardization: consistent workflows across shifts.
8.2 Trade-offs and risks
- More points of failure: cables, settings, permissions, storage, network.
- Training is mandatory for daily users.
- Governance required when recording/export is enabled.
- Maintenance cannot be “zero” if you want stable daily use.
8.3 Under poor maintenance / low-skill operation
- “No signal” events become frequent.
- Recording failures happen quietly (storage full, wrong profile, permissions, incorrect time).
- UI instability (overheating, dust, aging storage, poor power, no updates).
- Export chaos (privacy risk, missing files, wrong folders).
- Workarounds: staff revert to phone photos or standalone recorders.
8.4 Practical mitigations
- One-button defaults + locked presets.
- 2-minute daily check: signal → record test → storage → time.
- One named owner (biomed/IT/OR lead) with monthly checks.
- Small spare kit (key cables + storage module + critical adapters).
- Signal check: Confirm the main surgical display shows the default source (endoscope) with normal color/brightness.
- Switching check: Switch once to a secondary source (patient monitor / C-arm) and switch back.
- Recording test (10 seconds): Start recording → wait 10 seconds → stop → confirm the file appears in today’s folder.
- Storage check: Confirm free space is sufficient (avoid “silent failure” when storage is full).
- Time check: Confirm date/time is correct (wrong time creates messy case folders and audit issues).
9) Common Mistakes (and how to avoid them)
- Over‑specifying 4K everywhere: decide which sources truly need it.
- No acceptance test script: if you can’t test it, you can’t maintain it.
- Ignoring data policy: export rules must be agreed before go‑live.
- Assuming PACS is easy: confirm early; stage integration.
- Underestimating training: training is part of system stability.
10) How to Choose the Right Scope
Use these questions to lock scope without getting lost in IT terms.
- Which sources must be shown? (endoscope, vitals, field cam, C‑arm…)
- How many displays are needed—and where?
- Do you need 4K for every source or only specific ones?
- Will you record? If yes: who owns the files, who can export?
- Teaching room now or later?
- PACS/HIS integration Day 1 or Phase 2?
- Who maintains it after handover?
11) Future Trends
- Better usability and safer defaults.
- More interoperability and clearer integration scope.
- Edge/offline-first designs for low‑IT hospitals.
- AI assistance likely in documentation/search (governance still critical).
12) Terminology Glossary
Short, plain-language definitions for non‑IT readers.
| Term | Meaning (plain language) |
|---|---|
| Digital OR / Integrated OR | Centralized OR video/info workflow: view, switch, record, share, manage. |
| Source | Any device sending video (endoscope, monitor, camera, C‑arm). |
| Routing / switching | Choosing which source goes to which display(s). |
| PIP / PBP | Picture‑in‑picture / side‑by‑side multi‑view. |
| Latency | Delay between real action and what you see. |
| PACS | Hospital image library (CT/MRI/X‑ray storage & access). |
| DICOM | Standard for medical images. |
| HIS / EMR | Hospital information / patient record systems. |
| HL7 | Hospital messaging standard. |
| Role permissions | Who can view/record/export/admin. |
| Audit log | Record of actions (e.g., exports) for accountability. |
| VLAN | Network separation method. |
| Scene preset | One-button preset for routing/layout/camera/device states. |
13) FAQ
Do we need strong IT to start?
No. Many hospitals start with room-level video + recording. PACS/HIS can come later.
Is 4K always necessary?
Not always. Decide where 4K changes clinical value.
Who should own the system after handover?
One named owner (biomed/IT/OR lead) should coordinate monthly checks, training refresh, and support escalation.
What is the simplest acceptance test?
Run the Section 7 workflows as a checklist: show sources → switch layouts → record → save → find → export (if allowed). Repeat twice.
14) Summary
A Digital OR is best understood as a practical workflow system: sources → routing → displays → recording → teaching, with clear ownership and governance. Technology matters, but daily success depends on usability, training, maintenance habits, and staged scope.
15) References & further reading
External pages for readers who want deeper vendor descriptions. Availability varies by country.
- Barco Nexxis (integrated digital OR AV-over-IP): barco.com
- EIZO OR Wall Panel (CuratOR): eizo-or.com
- KARL STORZ OR Integration (OR1 portfolio): karlstorz.com
- Richard Wolf core nova (control/operation): richard-wolf.com
- Stryker OR Integration: stryker.com